What’s inside our Impact Report
Our Impact

127,000
People reached by our Voices of IBD campaign to make IBD more visible
3million
Visits to our educational webpages in 2023

31,000+
Members of our advocacy network who are fighting for health insurance reform, public restroom access, and more

945
Young people who found fun, friends, and support at Camp Oasis, our life-changing summer camp for kids and teens with IBD

$500million +
Money we've invested in research to date
1,600+
Scientists, clinicians, and industry leaders who attended our Crohn's & Colitis Congress
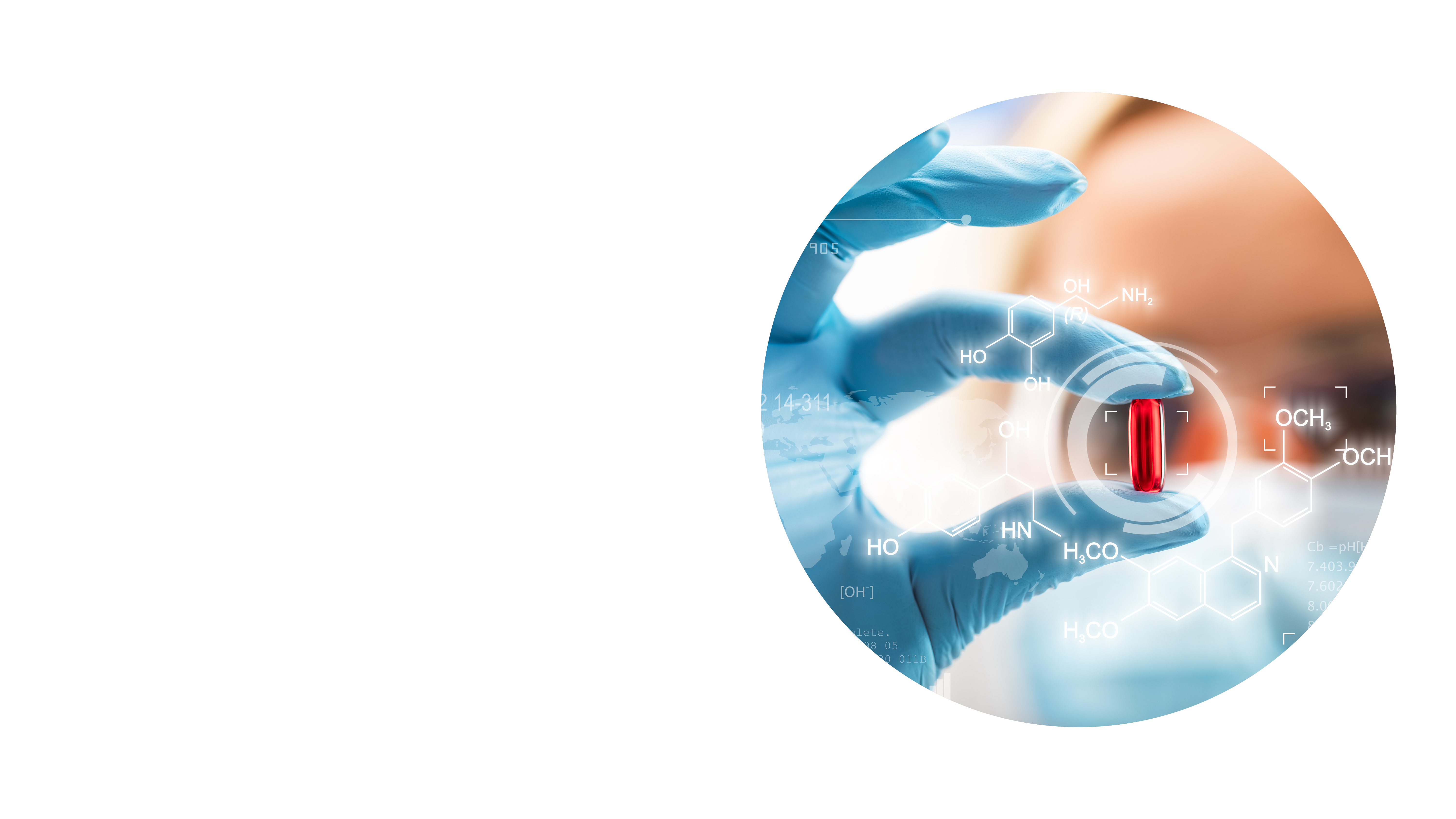
Our New Chief Scientific Officer
Crohn's & Colitis Foundation has welcomed Alan Moss, MD, as our new Chief Scientific Officer. He previously served as Director of the Crohn’s & Colitis Program at Boston Medical Center (BMC) and Professor of Medicine at Boston University (BU). Alan's experience as a doctor, researcher, and patient advocate, will drive our mission to accelerate the discovery of new and innovative therapies for IBD.
Learn more about Alan's vision for the future of IBD research and his advice for how patients can partner with their doctors on their care.
We’re seeing people have a lot more treatment options and we’re creating opportunities to personalize their treatment.
New Research Sheds Light on Stress-Related Flares
Like many patients, Katy Weniger says that stress goes hand-in-hand with her ulcerative colitis symptoms. “I consider it my number-one trigger, even more than diet,” she says. “When my stress level is really high, I start to flare almost immediately.”
For many years, both patients and clinicians have speculated about the impact of stress on IBD. Now, thanks to our vision and desire to support research in this area, we’re much closer to understanding why psychological stress has such an impact and what to do about it.
Using funding from our Environmental Triggers initiative, Emeran Mayer, MD, and his colleagues at the University of California determined that about half of ulcerative colitis patients studied relapse when exposed to stress. These individuals have elevated levels of several gut bacteria species as well as changes in blood and stool metabolites. Functional MRI studies are ongoing to identify related brain changes.
Further research will aim to determine whether gut microbiome tests or even simple questionnaires can be used to flag vulnerable patients and whether behavioral interventions, such as mindfulness, can successfully stop flares in their tracks.
We are revolutionizing the understanding of the impact of psychological stress on IBD.
My goal as a researcher is to answer the questions patients ask me in clinic every day.
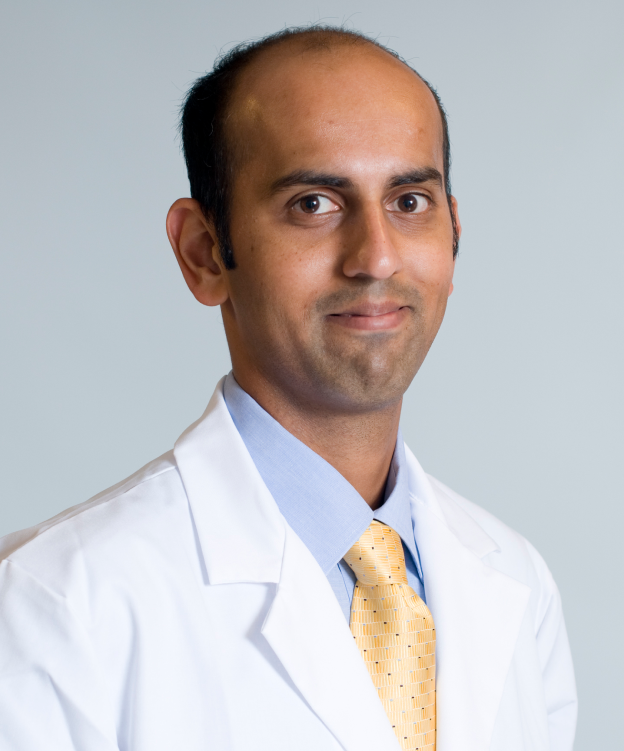
Translating Research to Personalized Care
Ashwin Ananthakrishnan, MBBS, MPH has devoted much of his career to bridging the gap between research and clinical care, and the Foundation is thrilled to have supported him along this journey.
When a patient tries a new medication, it’s a “coin toss” as to whether it will work. Using Foundation funding, Dr. Ananthakrishnan and his colleagues focused on improving those odds, demonstrating that it is possible to use microbiome analysis to predict whether a patient will respond to the drug vedolizumab (Entyvio) before they even take it. “The Foundation was instrumental in supporting this work,” he says.
The Foundation also provided funding for Dr. Ananthakrishnan’s research that linked microbiome changes to severe fatigue in patients whose disease is otherwise well-controlled. This paved the way for an ongoing study designed to assess whether probiotics can combat fatigue.
A physician investigator at Massachusetts General Hospital's Clinical and Translational Epidemiology Unit and associate professor at Harvard Medical School, Dr. Ananthakrishnan was recently named as one of Clarivate 2023 Highly Cited Researchers (see box, below). The Foundation has funded his research via our Senior Research Awards and Litwin IBD Pioneers program.
Congratulations to All the Clarivate 2023 Highly Cited Researchers!
Ashwin Ananthakrishnan, Harvard University
David Artis, Cornell University
Benoit Chassaing, Institut National de la Santé et de la Recherche Médicale
Jean-Frédéric Colombel, Icahn School of Medicine at Mount Sinai
Pieter C. Dorrestein, University of California, San Diego
Jeremiah J. Faith, Icahn School of Medicine at Mount Sinai
Jeffrey Gordon, Washington University in St. Louis
Wendy Garrett, Harvard University
Curtis Huttenhower, Harvard University
Nobuhiko Kamada, University of Michigan
James Lewis, University of Pennsylvania
Randy S. Longman, Cornell University
Dermot McGovern, Cedars-Sinai Medical Center
Long H. Nguyen, Harvard University
Bruce Sands, Icahn School of Medicine at Mount Sinai
William J. Sandborn, University of California, San Diego
Thaddeus Stappenbeck, Washington University in St. Louis
Harry Sokol, Sorbonne Université
Gary D. Wu, University of Pennsylvania
Ramnik Xavier, Broad Institute
Confidence, Independence, and Fun
Our research analyzing over 6,000 post-camp surveys completed by campers and caregivers over an 8-year period, revealed that campers benefitted from increased confidence and independence. They also made strides in feeling more comfortable in managing their IBD. Perhaps most importantly, they say that their camp experience makes them feel like they belong. Dr. Steven Steiner, pediatric gastroenterologist at Riley Children's Health Indiana and medical director at Camp Oasis, tells us about the significant of these findings.
“One of the most important takeaways is that pediatric IBD can be a very isolating disease, and Camp Oasis Michigan has proven to be a mechanism for patients—and their families—to overcome this barrier and continue the process of becoming young adults who can practice self-care more effectively.
“Most of my patients do not know a single other young person with IBD until they attend camp,” says Dr. Steiner. “Once there, a new circle of friends with a shared experience opens up to them.
“The data provides objective evidence of what all camp volunteers have observed—the multiple important ways that Camp Oasis influences young people living with IBD.”
Many kids are reluctant to talk about their disease or symptoms with people who are not familiar with the disease, given its sensitive nature. But when everyone at camp has experienced these symptoms, it becomes easy to easy to share, talk and bond.
Meet Riya Bahadur, Camp Oasis counselor
“I was diagnosed with ulcerative colitis during sixth grade. I missed a lot of school and felt like no one my age understood anything about me,” says Riya Bahadur, Camp Oasis counselor, former camper, and student at the University of California, Berkeley. “The first time I went to Camp Oasis I was very nervous, but that changed as soon as I arrived. I couldn’t believe that I could have conversations with other kids about my colon, being constipated, going to the bathroom—things that weren’t normal to talk about at home.”
Riya has returned to Camp Oasis every year and now she is a counselor. “Being a counselor for me is about giving back and giving other people the experience I had. The first thing I hear campers say when they get off the bus is ‘I want to see my friends.’ That’s what I like to hear.”
Camp Oasis is a Life-Changing Experience

98% of campers
shared that camp was a place they felt supported and a sense of belonging

Nearly 100%
of campers reported making at least one new friend, and most stayed in touch after camp

Almost 2 out of 3
new campers had never met another young person with IBD before camp

Down from 33% to 17%
the percentage of campers who reported feeling alone in their disease decreased after attending Camp Oasis
Making IBD Visible
IBD can be uncomfortable to talk about and is often called an “invisible disease.” Raising awareness of IBD is the goal of our Voices of IBD campaign, launched in January. To date, the campaign, which highlights the stories of IBD patients, providers, and Foundation staff, has reached 127,000 people.
Through this campaign, “IBD Warriors” like Lexi Comet have been sharing their experiences, and advice to help people understand IBD and give other patients a sense of hope and community.
“I am not ashamed of having Crohn’s disease and I refuse to stay silent,” says Comet. “Just by looking at me, people would have no idea that I battle an ‘invisible’ illness” each day of my life.”
The 2024 Crohn’s & Colitis Congress
In January, more than 1,600 scientists, clinicians, and industry leaders joined us in Las Vegas for the 2024 Crohn’s & Colitis Congress, the premiere IBD conference co-sponsored by the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
Highlights included a keynote presentation by Cedars-Sinai’s Stephan Targan, MD, on an exciting new treatment target (an inflammatory protein called TL1A); panel discussions on how IBD impacts other parts of the body, sometimes causing problems like arthritis; reports of new surgical strategies; and ample opportunities for brainstorming and networking.
Congress is aimed at those with a professional stake in IBD, but our “patient reporters” Aaron Blocker and Maggie Tretton were on the scene and charged with bringing top highlights to other patients via a variety of social media platforms.
“It’s important for patients to know that so many people are working to help them by creating new drugs, tools, and approaches that could potentially have a huge impact on their lives,” says Blocker, who has Crohn’s disease and leads the Support For Crohn's Disease and Ulcerative Colitis community on Facebook.
Tretton, who also has Crohn’s disease and runs the LetsTalkIBD channel on YouTube, was impressed by the scientific advances that were presented as well as the patient-centered focus. “Being an IBD patient even five to 10 years ago is not what it is today, and there’s such a brighter future moving forward,” she says.
We bring together leading scientists, industry, academic centers, healthcare professionals, and patients from around the globe to advise and guide decisions on the most promising areas of IBD research to pursue.
New Educational Resources Reach Spanish-Speaking Patients
Spanish is the second-most spoken native language in the world, and the rate of IBD in Hispanic/Latino people is similar to that of non-Hispanic Whites. We launched our Spanish language microsite in 2021 and have since enriched the site with additional Spanish language resources. In November 2023, we launched a video that discusses preparation and recovery from surgery, and in January 2024 added a new video with basic information about what IBD is and its impact on the Hispanic/Latino community.
“We want to make sure we’re addressing all parts of the IBD journey, as well as including information that is culturally relevant to the experience of native Spanish speakers,” says Catherine Soto, associate vice president of Patient Education & Support at the Crohn’s & Colitis Foundation.
Valery Vilchez Parra, MD, Explains Surgical Options for IBD to Spanish Speakers
La Dra. Valery Vilchez Parra nos proporciona una introducción a diversos tratamientos quirúrgicos para pacientes con enfermedad de Crohn y colitis ulcerosa.
YOUR SUPPORT MATTERS
All year, you participate in our community events and encourage us with your stories of hope and resilience. You inspire us with your commitment to raising funds that support IBD research, awareness, and initiatives designed to make the lives of people with IBD better. We invite you to continue your efforts and find your community of support through local events like our galas, Take Steps, Team Challenge, spin4 crohn’s & colitis cures, and more.
2022 Supporters
The following individuals and foundations have made important and significant contributions to the Crohn’s & Colitis Foundation in support of our mission programs. We are deeply grateful to them for their extraordinarily generous gifts.
Past Impact & Annual Reports
Read about the advances the Foundation has made in the IBD space.
A Message from our Leadership
Our dedicated team at the Crohn’s & Colitis Foundation remains steadfastly focused on our mission to find cures and improve the lives of people living with IBD. We are proud of the critical role we’ve played in every major research breakthrough in IBD. This Impact Report shares our latest research on biomarkers and the progress we are making towards creating personalized treatments for IBD patients.
Eighty-five percent of people who have engaged with the Foundation say that we have positively affected their IBD journey. In this report, you will learn about our new resources for helping people navigate IBD and live a better quality of life. You will also meet patients, doctors, and researchers who share first-hand the impact that we have had on their lives.
We see great things on the horizon and are committed to further accelerating the progress we are already making. All we need is your support to help drive our next breakthrough.
With warm regards,

Michael Osso
President & CEO


Amber Backhaus
Chair, Board of Trustees